Bladder Neck Contracture
Expert Evaluation and Reconstructive Management
Bladder neck contracture (BNC) is a narrowing or scarring at the junction of the bladder and urethra that can obstruct urinary flow and significantly impact quality of life. It most commonly occurs after prostate surgery, such as radical prostatectomy or transurethral prostate procedures, and may be recurrent or difficult to treat.
Dr. Alex J. Vanni is a nationally recognized leader in reconstructive urology with extensive experience managing complex and recurrent bladder neck contractures, including cases associated with prior surgery, radiation therapy, and failed endoscopic treatments. Patients are referred nationally for his expertise in advanced reconstruction aimed at restoring durable urinary function.
Bladder Neck Contracture Educational Video
What Is a Bladder Neck Contracture?
The bladder neck is the narrow channel where the bladder connects to the urethra. A bladder neck contracture occurs when scar tissue forms and constricts this opening, creating resistance to urine flow.
BNC most often develops as a complication of:
- Radical prostatectomy
- Transurethral prostate surgery (TURP, laser procedures)
- Radiation therapy for prostate cancer
- Prior bladder neck or urethral surgery
Contractures may develop months to years after treatment and can progress or recur, especially after repeated interventions.
Symptoms of Bladder Neck Contracture
Common symptoms include:
- Weak or slow urinary stream
- Difficulty starting urination
- Straining to void
- Incomplete bladder emptying
- Urinary retention
- Recurrent urinary tract infections
Important: In some patients, BNC may coexist with stress urinary incontinence, particularly after prostate surgery, making management more complex.
How Is Bladder Neck Contracture Diagnosed?
Accurate diagnosis is critical to determining the most effective treatment strategy. Evaluation may include:
- Detailed surgical and treatment history (including prostate surgery and radiation)
- Urinalysis and urine culture
- Cystoscopy to directly visualize the bladder neck
- Imaging studies when appropriate to assess associated urethral disease
Defining the severity, length, tissue quality, and prior treatments is essential—particularly in patients with recurrent or radiation-associated contractures.
Treatment Options for Bladder Neck Contracture
Management depends on the severity of obstruction, number of prior treatments, and associated conditions such as incontinence or radiation injury.
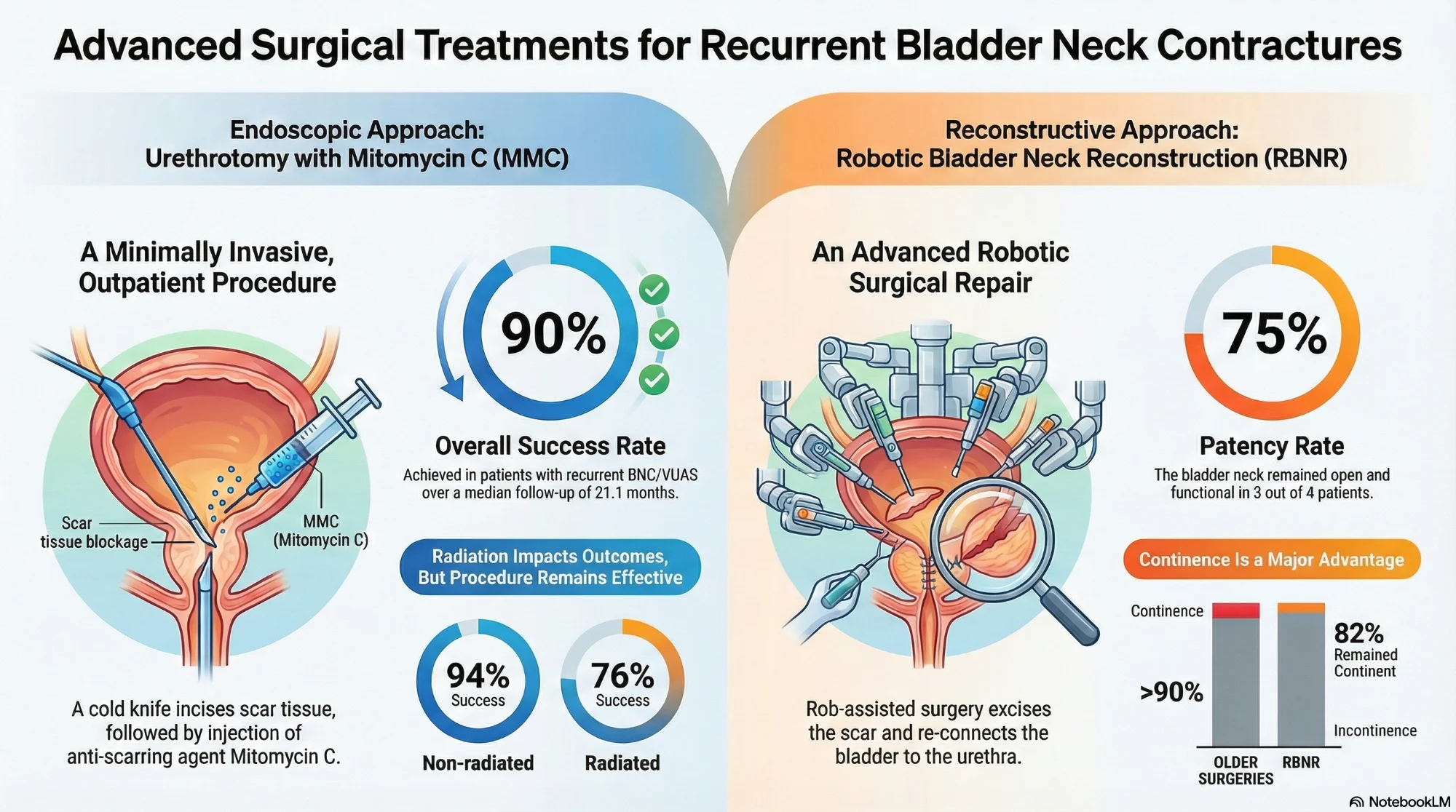
Endoscopic Treatments
- Bladder neck dilation
- Endoscopic incision or resection of the contracture
These approaches may be appropriate for select, early cases but are associated with high recurrence rates, particularly after repeated attempts.
Definitive Reconstructive Management
Patients with recurrent or complex BNC often benefit from evaluation by a reconstructive urologist with high-volume experience.
Dr. Vanni specializes in advanced surgical strategies, including:
- Open or robotic bladder neck reconstruction
- Reconstruction following failed endoscopic therapy
- Management of bladder neck contracture in the setting of prior radiation
- Coordinated planning when bladder neck obstruction coexists with urinary incontinence or requires future continence surgery (e.g., artificial urinary sphincter)
The goal of reconstruction is durable bladder neck patency, restoration of urinary flow, and thoughtful preservation or planning of continence.
Why Experience Matters in Bladder Neck Contracture Surgery
Bladder neck contracture surgery is technically demanding, particularly in patients with:
- Multiple prior endoscopic treatments
- Prior pelvic radiation
- Dense fibrosis or obliterative disease
- Concomitant urinary incontinence
Outcomes depend heavily on surgeon experience, careful patient selection, and individualized surgical planning. High-volume reconstructive centers are better equipped to manage these complexities and minimize the need for repeated procedures.
Dr. Vanni's outcomes reflect a commitment to technical excellence, patient safety, and long-term durability—especially in patients with challenging or recurrent disease.
National Referral Center for Complex Bladder Neck Contracture
Patients with refractory bladder neck contracture are referred nationally to Dr. Vanni for expert consultation and definitive management. He works closely with referring urologists to ensure coordinated care, clear communication, and long-term follow-up.
Have Questions About Bladder Neck Contracture?
Get answers to the most common questions about bladder neck contracture treatment, surgery, and recovery.
View Frequently Asked QuestionsDr. Vanni's treatment protocols are grounded in peer-reviewed evidence and current AUA guidelines for the management of bladder neck contracture.
Treatment Outcomes at a Glance
Success Rate
76–94% success with endoscopic treatment; 75–90% with robotic reconstruction
Surgery Duration
1–3 hours depending on approach
Recovery
Most patients recover within 4–6 weeks



Schedule a Consultation
If you have persistent urinary obstruction after prostate or bladder surgery—or have undergone multiple unsuccessful treatments for bladder neck contracture—expert evaluation can help determine the most effective next step.